Obstructive sleep apnea is a serious breathing problem that interrupts your sleep.
Obstructive sleep apnea (also called OSA or obstructive sleep apnea-hypopnea syndrome) means you have short pauses in your breathing when you sleep. These breathing pauses – called apneas or apnea events – last for 10 to 30 seconds, maybe longer. People with obstructive sleep apnea can stop breathing dozens or hundreds of times each night leading to sleep disruption and low levels of oxygen.
Obstructive sleep apnea stops you from having the restful sleep you need to stay healthy. If it’s not treated, sleep apnea can lead to daytime sleepiness, and reduced cognitive function. People with untreated obstructive sleep apnea have an increased risk of motor vehicle crashes, cardiovascular disease, hypertension and early death. Thankfully, there are excellent treatments for obstructive sleep apnea.
How obstructive sleep apnea affects your breathing
Obstructive sleep apnea stops you from breathing normally at night. If you have obstructive sleep apnea, you probably repeat this cycle while you sleep:
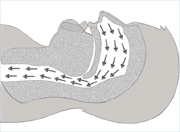
First, you may sleep quietly and breathe normally. The air in your airway (breathing tube) flows easily to your lungs.
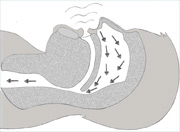
Then, you begin to snore loudly. This is a sign that your airway is partly blocked. If the blockage worsens this may affect the amount of air that can enter your lungs and your oxygen level can drop. (When doctos see this kind of drop in oxygen level due to a partially blocked airway in a sleep test, they call it a hypopnea.)
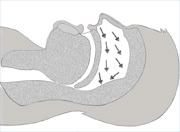
Next, your airway closes off completely. No air reaches your lungs. Your brain is telling you to breathe as usual, but you can’t take in a breath because your airway has closed off. This is called apnea. After a pause of 10-30 seconds or more, your brain realizes you haven’t been breathing, so it jolts you awake enough for you to take a breath. You take in a big gasp of air and start breathing again.
This cycle can continue through the night: you breathe quietly; you snore; you have a pause in your breathing; you gasp for breath; and you start breathing again. Most people have dozens or hundreds of sleep apnea events a night. This means dozens or hundreds of interruptions of sleep. You can’t get the restful sleep you need to be healthy.
The combination of both apnea events (pauses in breathing) and hyponea events (partly blocked breathing) is called obstructive sleep apnea-hyponea syndrome (OSAHS).
What can make a person’s airway collapse during sleep?
There are a few reasons why a person’s airway can partly or completely collapse during sleep:
- your throat muscles are too relaxed to hold your airway open
- you have a narrow airway.
- your tongue blocks your airway
- fatty tissue blocks your airway
Other types of sleep apnea
This website focuses on obstructive sleep apnea (OSA), the most common type of sleep apnea. There are three other types of sleep apnea: central sleep apnea, mixed or complex sleep apnea and sleep-hypoventiation syndrome.
Who’s most at risk for obstructive sleep apnea?
Anyone of any age can get obstructive sleep apnea. Your risk is higher if you have a combination of these risk factors:
- You’re obese (very overweight).
- You have a large, thick neck (larger than 17 inches for men; larger than 16 inches for women).
- Your family has a history of obstructive sleep apnea.
- You’re male.
- You’re older than 40.
- You have large tonsils.
- You have a recessed chin (your chin tucks in).
Children are at higher risk of sleep apnea if they have large adenoids and tonsils. Tonsils and adenoids are tissues in the back of the throat. You can see tonsils by looking into the mouth. You can’t see adenoids – they are higher up in the throat.
Taken from the Lung Association of Canada. This content was reviewed on October 15th, 2014 by The Canadian Thoracic Society’s Sleep Disordered Breathing Clinical Assembly.




